Before you freak out and throw away your pills, you’ll probably want to read this.
There’s been A LOT of talk about birth control raising your risk of blood clots, especially some of the newer kinds.
Monik Markus / Creative Commons / Via Flickr: 42954113@N00
This probably isn’t news to most people — it’s a well-known side effect that’s been in the prescription information forever. And in the past few years, more and more studies have looked at the risk of blood clots associated with newer birth control options, like the ring, the patch, and oral contraceptives with new kinds of progestin (like Yasmin or Yaz, which contain the progestin drospirenone).
SO here’s what you need to know about your blood clot risk and how it’s impacted by which birth control you use:
Here’s what a blood clot actually is:
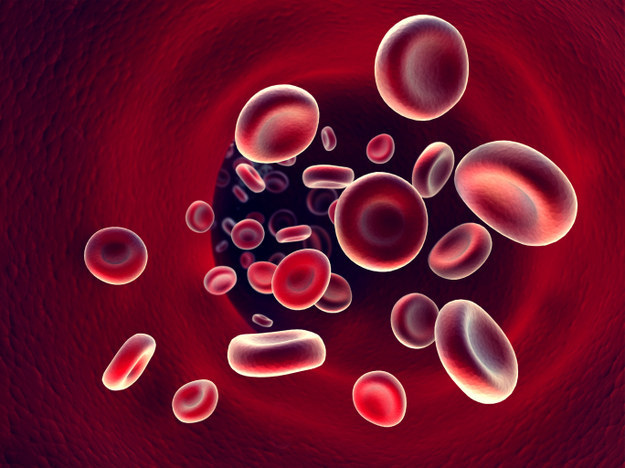
Andriy Muzyka / Getty Images / Via thinkstockphotos.com
When you get a cut or scrape, blood clotting is a normal thing that happens to stop the bleeding. But when a clot forms in a vein or artery, it can be dangerous and sometimes fatal. Blood clots in veins are called venous thromboembolism (VTE), which refers to two different kinds of clotting complications and affects about 300,000 to 600,000 people in the U.S. each year. Deep vein thrombosis (DVT) is when a clot forms in a major vein (like in your legs, arms, or pelvis). Pulmonary embolism (PE) is when a clot detaches and travels to the heart or lungs, where it cuts off blood flow.
Doctors aren’t always sure what causes a clot, but there are some things that can raise your risk of developing one.

ABC / Via wifflegif.com
Some of the main risk factors for VTE are major surgery, being hospitalized for an acute illness, immobility, cancer, obesity, and trauma to your legs, ankles, hips, or pelvis, Dr. John Heit, professor of medicine in the Division of Cardiovascular Diseases at Mayo Clinic, tells BuzzFeed Life. For women, the risk of clots is also higher during pregnancy, right after giving birth, when taking hormone therapy, and when taking many types of hormonal birth control. There’s also evidence that the risk of blood clots in veins is somewhat inherited, says Heit.
Yes, being on some kinds of birth control can slightly raise your risk of blood clots. But not all of them.
The best evidence shows that the estrogen and progestin in birth control increases the concentration of blood clotting components, which increases the risk of developing a clot, says Heit. However, the hormonal and copper IUDs have not been shown to increase your risk, says Gunter.
So what about this new study that says newer birth controls give you a 4x higher risk of blood clots?! OK… let’s talk about that.

Fuse / Getty Images / Via thinkstockphotos.com
The study results — which have been making terrifying headlines this week — found that your risk of getting a blood clot is 1.8x higher if you take birth control with a newer form of progestin than if you take birth control with an older form. They also found that the risk of a blood clot on these newer pills is up to about 4.3x higher than if you don’t take any birth control at all. Again, that sounds terrifying. The problem is, most reports aren’t actually explaining what those numbers mean and giving them context – like, you know, how many people actually get blood clots… and 4.3x higher than what?!
BuzzFeed Life spoke with the lead study author Yana Vinogradova, research statistician at the University of Nottingham, to find out more about the study, which you can read in full here. They compared the blood clot risk associated with different types of progestin, the synthetic hormone found in some types of birth control. One of the most common progestins is levonorgestrel (found in some birth control pills, Plan B One-Step, and the hormonal IUD). But this study also looked at newer types of progestin like drospirenone (found in Yasmin or Yaz) and desogestrel (found in Desogen or Mircette).
So here’s what those numbers ~actually~ mean:
Warner Bros. / Via reddit.com
Based on their estimates, the rate of blood clots while not on any birth control is 4.2 per 10,000 women in a given year. (Heit and Gunter confirm that about 3-5 women per 10,000 will get a blood clot each year.) So that’s a 0.04% chance of getting a blood clot. Very small chance, but it happens.
For women taking a levonorgestrel-containing birth control pill (an older one), they estimated that 6 extra cases per 10,000 women would occur each year. For women taking a drospirenone-containing pill, they estimated that 13 extra cases per 10,000 women would occur each year; and for women taking a desogestrel-containing pill, they estimated 14 extra cases per 10,000 women. So we’re basically looking at a difference between 0.04% chance and 0.18% chance.
“Even though the risk is slightly increased, it’s still very low,” says Heit. So what causes this difference? It’s thought that the estrogen in birth control is what mostly accounts for this overall increased risk, and the newer types of progestin might also directly affect the clotting mechanism or they might impact estrogen in a way that affects your clotting, says Gunter.
Ready to have your mind blown? Your risk of getting a blood clot is 4-5X higher when you’re PREGNANT, and it’s 20X HIGHER in the postpartum period.

Jerry Lai / Creative Commons / Via Flickr: jerrylai0208
So, yeah, even the newer birth control pills can’t compete with that risk. Your risk of having a blood clot while on newer types of birth control is still lower than your risk of having a blood clot during pregnancy or the postpartum period, confirms Vinogradova. So before you throw out your pill, keep in mind that getting pregnant would up your risk even more. Basically, all those fear-mongering headlines are absolutely terrifying, but they’re not telling the whole story.
And obviously there are limitations to this (and every) study that you should keep in mind.
In case you’re curious, here’s a little more info about how they got these estimates: The researchers pooled data from two large medical databases in the U.K., and they looked at women between the ages of 15-49 who were diagnosed with VTE between 2001 and 2013. This gave them over 10,000 VTE cases to look at. Then they compared each of these cases with 5 control cases (women who were the same age and in the same medical practice who did not have VTE.) Controlling for BMI, smoking status, alcohol consumption, and other common confounding variables, they used statistical models to estimate how much more likely someone was to have a blood clot when taking the newer forms of progestin.
Their results are similar to what other researchers have found in the past: a slightly increased risk of blood clot while taking newer forms of progestin. That said, it’s hard to look at any of these studies and find conclusive cause-and-effect data, because these are estimates, and even though they controlled for many variables, there are plenty of limitations. For example, this study only looked at one year of prescription records, so it’s possible that the non-pill users actually were on birth control in the past. It’s also possible that the ones on the newer pills had already tried several others in the past before settling on their current method. It also could be the case that when these newer pills came out, doctors may have put their higher risk patients on them, because they were touted as being the next great thing, says Gunter. Basically, there’s still a lot we don’t know.
So should you switch your birth control or stop taking it completely?
If you’re in good health and are a good candidate for birth control, don’t freak out over this new study. “Think about this as the worst case scenario,” says Gunter. “And you assume a risk when you take any kind of medication.” It’s also important to keep in mind that this heightened risk would be most relevant in your first year on birth control (since that’s when your body is getting used to the hormonal differences), says Gunter, and your risk will go back to normal once you stop taking it.
But if you have other factors that could put you at a higher risk of complications (like a personal or family history of clots, smoking, obesity, cardiovascular disease, migraines with aura, or you’re over 35), talk to your doctor about what birth control option would be best for you. These aren’t all signs that you can’t take birth control, but several little factors may add up to an increased risk of clots or stroke, so talk to your doctor if any of them apply to you. They may suggest a method without estrogen (like the minipill or the hormonal IUD) or one without any hormones (like the copper IUD or condoms).
And if you’re just now considering birth control, it’s always a good idea to ask your doctor for the lowest-dose and lowest-risk option that will still give you the protection and the benefits that you need, says Gunter.
One last thing! Here are the signs and symptoms of a blood clot, just so you know:

Dirima / Getty Images / Via thinkstockphotos.com
The symptoms of DVT in the leg often include pain, swelling, and redness usually in the calf or ankle, says Heit. It may also feel hot to the touch or feel painful behind your knee. A clot in another vein may lead to swelling and pain in other areas, but those are less common. The symptoms of PE (when a clot moves to your lungs) include shortness of breath, chest pain, rapid heartbeat, and feeling faint. Of course, these symptoms could come from a number of things, but if something feels really off, definitely see a doctor, says Heit.

















