Almost 200,000 unplanned pregnancies occur in Australia each year, though not all go full term. Safe and effective emergency contraception is necessary to help prevent unintended pregnancies in people who do not wish to fall pregnant.
Until 2015, the levonorgestrel “morning after pill” (for example the common brand name Postinor®) was the only oral emergency contraception available in Australia. It comes as one 1.5mg tablet or two 0.75mg tablets and is available from a pharmacist without a prescription from A$14.99.
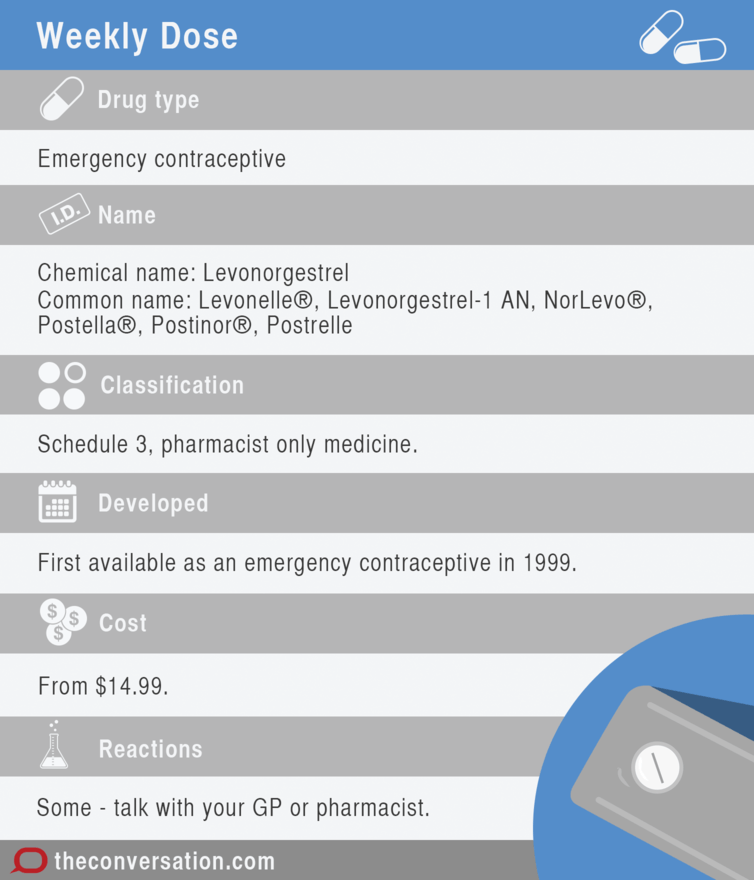
Now a new option, EllaOne® (ulipristal), is available in Australia with a doctor’s prescription. But how are they different, and which one should you choose?

How does it work?
Levonorgestrel is a synthetic progestogen, which is a drug used to mimic the effects of the body’s own hormone, progesterone (a sex hormone involved in the menstrual cycle and pregnancy). It is thought to work by inhibiting or delaying ovulation, and impeding transport of sperm and/or egg to prevent fertilisation. It may also change the uterus environment to make it more difficult for a fertilised egg to attach to it.
Last year the Therapeutic Goods Administration approved ulipristal (EllaOne), which has been used as emergency contraception in the European Union (EU) since 2009. Ulipristal was approved to treat uterine fibroids (common benign growths) in Canada in 2013 and the EU in 2015. However this was a 5mg dose, much lower than the 30mg emergency contraception dose.
EllaOne is an oral tablet (30 mg) that is taken as a single dose and is currently only available on prescription in Australia. EllaOne does not yet have a recommended retail price (RRP) in Australia, however, its RRP in the United Kingdom is £34.95, or almost A$70.
Ulipristal was developed from a molecule similar to progesterone and binds more strongly and more specifically to the progesterone receptor compared to levonorgestrel. Ulipristal blocks the effect of the body’s progesterone, inhibiting or delaying ovulation. It may also make it more difficult for a fertilised egg to attach to the uterus.
For emergency contraception, both levonorgestrel and ulipristal should be taken as soon as possible. However, while levonorgestrel should be taken within 72 hours, ulipristal should be taken up to 120 hours (five days) after unprotected sex or contraceptive failure. Contraceptive failure can be missing a regular active contraceptive pill, or having used a broken condom.
Side effects
Clinical trials found levonorgestrel and ulipristal had comparable side effects. These were mild to moderate in nature, short-lived and resolved on their own. The most common side effects reported were stomach aches, nausea, and headaches.
Both levonorgestrel and ulipristal are metabolised and broken down by a specific liver enzyme called cytochrome P450 3A4. The effectiveness of these medications may be reduced when taken with other medicines that increase the activity of this liver enzyme (such as St Johns Wort and some epilepsy medicines).
Women who require emergency contraception because they missed a regular active contraceptive pill should resume taking their normal pill within 12 hours after taking levonorgestrel. However, ulipristal may reduce the effect of any contraceptive pill that contains a progestogen (synthetic progesterone).
Consequently, EllaOne’s manufacturer recommends waiting at least five days before the regular contraceptive pill is restarted. During this time, barrier methods of contraception (such as condoms) are recommended until cover from the regular contraceptive pill is achieved, so this can be up to one week after recommencing, or almost two weeks after taking EllaOne.
So which is more effective?
Levonorgestrel is most effective when taken within 24 hours after unprotected sex as it prevents 95% of expected pregnancies. After 24-48 hours, the effectiveness decreases to 85%, then 58% after 48-72 hours. Ideally it is taken within three days as the benefits after 96-120 hours are uncertain.
When used within 72 hours, ulipristal is linked to lower pregnancy rates compared to levonorgestrel. This effect is maintained up to 120 hours afterwards. However, ulipristal is not effective after ovulation, which usually occurs in the middle of each menstrual cycle.
The data from clinical trials shows that within 72 hours of unprotected sex, there is a slightly lower risk of becoming pregnant with ulipristal than levonorgestrel. Ulipristal has some evidence to support use up to 120 hours after unprotected sex. So it is slightly more effective than levonorgestrel up to 72 hours; and can work up to 120 hours. It is important to remember – the longer you wait after unprotected sex, the less effective either option is.
Women need to weigh up all these factors to make a decision for their circumstances. These can include the slightly higher efficacy of ulipristal, whether or not they have ovulated, accessibility (without prescription from a pharmacy or needing to see their GP), the time elapsed since unprotected sex and cost.
It is also worth remembering there is no easy test from the GP surgery or pharmacy to determine if ovulation has already occurred. This means ulipristal could be a waste of time, while levonorgestrel may still provide some protection.
The decision is not easy to make and the available information does not provide a clear solution. Each woman will have multiple factors that provide a unique mix, so it is not possible to provide blanket advice on a preferred option. Women requiring emergency contraception should discuss the matter with their GP or pharmacist.
![]()
Esther Lau is affiliated with the Pharmaceutical Society of Australia.
Lisa Nissen is affiliated with Pharmaceutical Society of Australia (QLD branch committee) Member of the QUM advisory board for Abbvie – Hepatitis C
Greg Kyle, Jose Manuel Serrano Santos, and Yasmin Antwertinger do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond the academic appointment above.


















