If you plan on having kids one day, here are some things you should know.
Sashkinw / Getty
Maybe you’re actively trying to conceive a child. Or maybe you are pretty sure you want kids down the line. Or maybe you just want to keep your options open.

Rayes / Getty Images
If any of those apply to you — whether you’re a man or a woman, cisgender or transgender — here’s what you have to know about how sexually transmitted infections (STIs) play a role in your future fertility.
First things first: Understand that everything we’re about to tell you is meant to inform you, not totally freak you out. STIs can sometimes make it harder to get pregnant naturally, but that doesn’t necessarily mean you’ll never have babies.
This is so important.
We’re breaking this post apart into three sections:
1. STIs & Fertility — the basic facts about which STIs do what.
2. How To Protect Yourself — how to keep yourself and your fertility safe.
3. If You Want To Have A Baby — what to do if you’ve had any of these STIs and are trying to have a baby, or want to have a baby at some point in the future.
If any of this stuff applies to you and you want to have kids (even five or ten years down the line!), you should have a conversation about it with your doctor. They can help you assess your risk, and you can work together to come up with a plan that makes sense for you, based on your personal history.
OK, now let’s get into it.

CK
What you need to know.
Chlamydia and gonorrhea could potentially hurt your future fertility, regardless of your gender.
For cisgender women and transgender men, gonorrhea and chlamydia can potentially cause scarring and damage to the fallopian tubes.
This is why it’s so important to get tested if you’re at risk for STIs — and get treated ASAP if you happen to contract one. The sooner you can treat and cure chlamydia or gonorrhea, the less likely they are to cause damage to your reproductive organs.
Another reason to stay on top of your screening and treatment: In cases where these infections go unnoticed or untreated for long enough, they can migrate further into the pelvis and cause pelvic inflammatory disease (PID). “By the time PID happens, significant damage has happened to your tubes,” Dr. Lubna Pal, reproductive science specialist, OB-GYN, and director of the Polycystic Ovary Syndrome Program at the Yale University School of Medicine, tells BuzzFeed Life. Additionally, if you have PID once, you’re at a greater likelihood of developing it again.
For cisgender men and transgender women, gonorrhea and chlamydia can potentially damage your pipes as well, although it’s very rare, and much less common than fallopian tube damage.
“The male reproductive tract — the urethra and the ejaculatory duct — can be affected by STDs like gonorrhea and chlamydia; they can be scarred, which causes an obstruction,” Dr. Thomas Molinaro, a reproductive endocrinologist at Reproductive Medicine Associates of New Jersey (RMANJ) in Eatontown, tells BuzzFeed Life. “It’s definitely less prevalent than gonorrhea or chlamydia affecting fallopian tubes in women, but it is still something that we see and that men should be aware of.”
Scarring or damage to the fallopian tubes can cause what is referred to as “tubal infertility.”
Scarred and damaged fallopian tubes can prevent sperm from reaching and fertilizing the egg. And if an egg does get fertilized, blocked tubes can also keep that fertilized egg from reaching the uterus. This can increase your odds of having an ectopic pregnancy — when the embryo implants in the fallopian tube wall, rather than in the uterus wall. Ectopic pregnancies are completely nonviable, and they’re very dangerous — and can even be fatal.
If you have a penis and your urethra and ejaculatory duct are blocked, it can prevent you from actually releasing sperm.
STI-related damage obstruction in men is rare, but not unheard of. “I’ve seen patients who have an inability to release the sperm; the outflow tract is scarred down from previous STIs,” Molinaro says. “There are some surgeries that can be done, but oftentimes when you have an obstruction like that, it requires testicular biopsy to get sperm.” Not so fun.
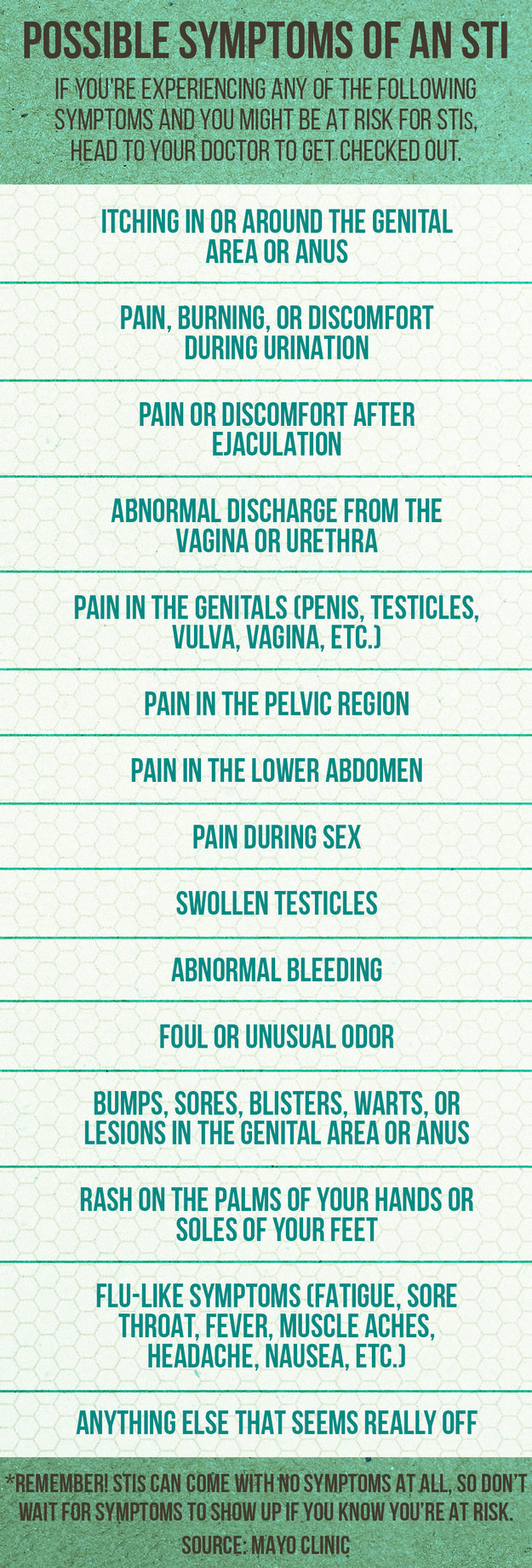
Chlamydia and gonorrhea often have absolutely no symptoms at all, so you might not even realize you’re infected.
This is why it’s incredibly important to get tested and know your status — the longer you’re infected with chlamydia or gonorrhea, the greater the likelihood that these infections can damage your tubes. It also means that you might inadvertently infect your partner, impacting THEIR future fertility as well.
HPV won’t harm your fallopian tubes in the same way that chlamydia and gonorrhea can — but certain treatments could make it harder for you to get pregnant or carry a baby to term.
HPV (human papillomavirus) is the MOST common STI in the United States: More than half of all sexually active people are believed to contract it at some point in their lives, according to the National Cancer Institute. Most of the time, the HPV will go away naturally on its own within about two years. But some strains of HPV don’t go away so easily for some people, and a few really bad ones can cause cancer.
If a pap smear and colposcopy reveal that you have pre-cancerous cells on your cervix, your doctor might need to perform a procedure meant to cut those cells out. Some of those procedures, such as LEEP biopsies, cone biopsies, and cryotherapy, can pose a small risk of harming your fertility, Pal says. There’s a risk that the biopsy might change your cervix in a way that you no longer produce enough cervical mucus — which can make it harder for the sperm to get to where they need to go. In other cases, where the biopsy cut is especially large, it could compromise your cervical integrity, upping your risk of miscarriage once you do get pregnant. It’s also worth noting that if you actually end up developing cervical cancer (rather than just pre-cancer), certain treatments for that can also pose a risk to your fertility.
All that being said: Absolutely do not freak out if you’ve had these procedures or have been advised to get them done. There are definitely things that your doctor can do to help improve your chances of getting pregnant down the line, and there’s a simple procedure that can help you carry your baby to term if you have trouble with cervical integrity. More on that in section three.
Herpes, syphilis, and trichomoniasis also don’t hurt your tubes in the way that chlamydia and gonorrhea can.
That said, herpes can absolutely be a problem if you have an outbreak when you’re giving birth. “If there’s an active herpes infection at the time of delivery, the mom needs a C-section to prevent the herpetic shedding to the baby,” Dr. Jane Frederick, specialist in reproductive endocrinology and infertility, and medical director of HRC Fertility in Orange County, California, tells BuzzFeed Life.
If you’ve ever been diagnosed with ANY STI, it could still be a sign that you’ll have a hard time conceiving down the line — even if the STI wasn’t specifically chlamydia or gonorrhea.
That’s because many STIs tend to happen at the same time as each other. So if you have herpes, there’s a high likelihood that you’ve ALSO been exposed to gonorrhea. “It’s not about only one infection that’s bad and everything else is OK,” Pal says. “It’s more like a peer group that tends to cohabitate — one infection tends to [happen concurrently] with another.”

CK
How to keep yourself and your fertility safe.
You can lower your risk of contracting chlamydia and gonorrhea by practicing safe sex.
What this means: Unless you’re in a mutually monogamous relationship where you and your partner have both tested negative for all STIs, you should use a condom or barrier method every time you have sex, whether it’s vaginal, anal, or oral. Condoms aren’t 100% effective — they can break, for instance, and some infections, like HPV, can be transmitted from skin-to-skin contact that isn’t always covered by a condom. But they can definitely help prevent the spread of chlamydia and gonorrhea, and they’re absolutely better than going without.
Oh yeah — and let’s say you forgot to use a condom once or twice. That doesn’t mean you should just give up and stop using condoms altogether. Using condoms most of the time is better than none of the time.
You should make sure that you know your STI status by getting tested when necessary.

Alice Mongkongllite / BuzzFeed / Via
Here’s a basic checklist for whether or not you need to be tested, based on CDC guidelines and interviews that BuzzFeed Life conducted with sexual health experts. For more (extremely detailed) information about when you should get tested and for what, .
Chlamydia and gonorrhea are TREATABLE diseases — and the sooner you detect them, the sooner you can get treated for them.
Chlamydia and gonorrhea are both bacterial infections, which means that they can almost always be treated with antibiotics. If you or your partner are diagnosed with chlamydia or gonorrhea, make sure that you take doctor-prescribed antibiotics to treat the infection ASAP. The sooner you get treated, the less likely they are to cause damage to your reproductive organs.
You can also be treated for PID.
Your doctor will prescribe antibiotics to treat cases of PID, but as with chlamydia and gonorrhea, it’s super important to address it quickly. The longer you go untreated, the more damage it can cause.
Alice Mongkongllite / BuzzFeed / Via
When you’re taking antibiotics to treat an STI or PID, take the entire course of antibiotics.
This is so important: DON’T STOP taking antibiotics just because you feel better. You can stop experiencing symptoms before the infection has been totally eradicated, which means that it can still cause problems for you.
If your partner has an STI, make sure they get fully treated. And you should also be treated as well.
In some states, doctors who diagnose one partner with an STI will write a scrip for the other partner without even seeing them. That’s because it’s incredibly likely that if your partner has an STI, you’ve been exposed and should be treated as well. If you don’t live in one of those states, be sure to get tested and treated right away if your partner has an STI.
And if you’re the one with the STI, tell your partner right away so they can get the treatment they need, and so that you don’t just pass the infection back and forth to each other.
http://mtvitsyoursexlife.tumblr.com/post/109612992341/3-this-more-on-condoms-here
You can and should get vaccinated against HPV, if you aren’t already.
Getting vaccinated against HPV at a young age is the best protection you have against contracting HPV and developing HPV-related cancers. The CDC Advisory Committee on Immunization Practices recommends that all females and males at ages 11 and 12 get vaccinated, although you can choose to have your kids vaccinated as young as 9 years old. Everyone can and should get vaccinated by the time they’re 26.
“I’m encouraging moms and dads to get their children vaccinated while they’re preteens,” Frederick says. “That’s the only vaccine we have right now to prevent cancer.”
In the meantime, if you have a vagina make sure that you are getting pap smears on schedule as recommended by the CDC, to catch abnormal cells early before they become more advanced or turn into cervical cancer. Unfortunately there is no approved HPV test for cisgender men or transgender women, so it’s especially important for cisgender women and transgender men to stay on top of their own health and get screened at the recommended times. Find out .
If you are diagnosed with cervical cancer, you should talk to your doctor about potential fertility-preserving treatment.
Advanced-stage cervical cancer treatments — like radiation, or surgery to remove the cervix and uterus, for example — can affect your fertility in ways that are unfortunately unavoidable. But if you have very early-stage cervical cancer, it might be possible to get a procedure called a radical trachelectomy, which can potentially preserve your fertility. Again, speak with your doctor about your options, and be sure to seek a second opinion about your best options for treatment if you are ever facing a cancer diagnosis.
CK
Here’s what to do.
Get tested for STIs.
Find out if you’re currently infected with anything. If you are, get treatment ASAP.
Talk to your doctor about any STIs you’ve ever had, even if you’ve never had chlamydia or gonorrhea.
Again: Exposure to one STI increases your risk for exposure to others — so even if you’ve never been officially diagnosed with chlamydia, you still might have contracted it at some point in the past. Because potential damage to your tubes increases your risk of ectopic pregnancy, your doctor might want to keep an eye on you during your efforts to get pregnant, as well as tell you what to watch out for.
Typically, fertility experts recommend that if you’re under 35, you should try to conceive for a year before seeking fertility treatment. But if you have a history of STIs (particularly chlamydia or gonorrhea), your doctor might tell you to try for six months before coming in for testing. They might also suggest you get certain tests before you even start trying. These recommendations will differ depending on your personal circumstances, as well as other health, lifestyle, and family history factors, so again: Communicate with your doctor, and work together to come up with a plan that makes sense for you.
If you’ve ever had chlamydia, gonorrhea, or PID, your doctor might want to perform a test to check to see if your fallopian tubes are blocked.
For instance, they can perform an ultrasound test or an X-ray test to check for blockages. That said, these tests don’t give you the all-clear, and even if your test comes back saying your tubes aren’t blocked, it doesn’t mean pregnancy is going to be easy — “The X-ray can tell you if your tubes are open, but they can’t tell you if your tubes are working well,” Pal says.
If you do have damage to your fallopian tubes, there are still things you can do to get pregnant.
When it comes to tubal damage, “in today’s day and age, the safest and most effective strategy is IVF [in-vitro fertilization],” Pal says. IVF is when your doctor extracts eggs from your ovaries, fertilizes them with sperm in a lab, and then injects them back into your uterus — bypassing your fallopian tubes altogether.
IVF can be incredibly expensive, and it’s possible that your insurance won’t cover the costs. But that’s why educating yourself about your options and your situation is important: “It’s about planning,” Pal says. “If a 22-year-old knows her tubes are blocked because she had PID, maybe she can plan and save, or find the best insurance.”
If you have blocked fallopian tubes, you should talk to your doctor about your options.
If you’ve ever had a LEEP biopsy or cone biopsy to take care of pre-cancerous cells on your cervix, your doctor can examine your cervix and figure out the best course of action.
If your cervical mucus production has been affected, you might want to try intrauterine insemination, Pal says. That’s when your doctor inserts the sperm directly into your uterus (bypassing the cervix) using a tiny soft plastic catheter.
If the issue is that you’ve had a cone biopsy or a deep cervical biopsy, that could increase your risk of miscarriage, because of “cervical incompetence,” Pal says, which basically means that your cervix might open up during your pregnancy. In this case, your doctor could perform a procedure called a cervical cerclage, where they basically stitch your cervix together, so it doesn’t open up too soon.
Even if you’re not planning to have kids NOW, you should still talk to your doctor about it in case you need to figure out a plan.
This advice is directed more toward cisgender women and transgender men: Your eggs decline in both number and quality the older you get. Once you reach your mid-thirties, that decline happens at a faster rate, and getting pregnant even under perfect conditions becomes less likely. To put it in perspective: A healthy 30-year-old has a 20% chance of getting pregnant during every menstrual cycle. A healthy 40-year-old has a 5% chance of getting pregnant each menstrual cycle. Your personal odds of getting pregnant will then also differ based on a number of factors: lifestyle habits (like smoking and drinking), your health, your menstrual cycle, your weight, your mother’s health and reproductive history, and more.
What this means is that if you’re thinking of putting off starting a family, you should definitely figure out if you have any complications that you might need to contend with. This way you’ll know if you might want to get started earlier than you originally hoped or planned, to give yourself enough time to conceive before things become even more difficult as you get older.
Ultimately, being informed about these issues at the outset can help you better plan for your future — emotionally, financially, and with your choices around timing. If you know that you might need a costly medical procedure down the line, for instance, you may start saving for it early. Or if you know that it might take you a bit longer than most people to get pregnant, you might want to plan to start trying a bit earlier. Things like that.
The bottom line: If you have any history of STIs at all, talk to your doctor about what your options are.
Don’t freak out, and don’t give up hope. There are often many different things you can do to help improve your odds of conception. The key is to communicate with your doctor and figure out what’s going on with enough time to take care of business.

Gianliguori / Getty Images